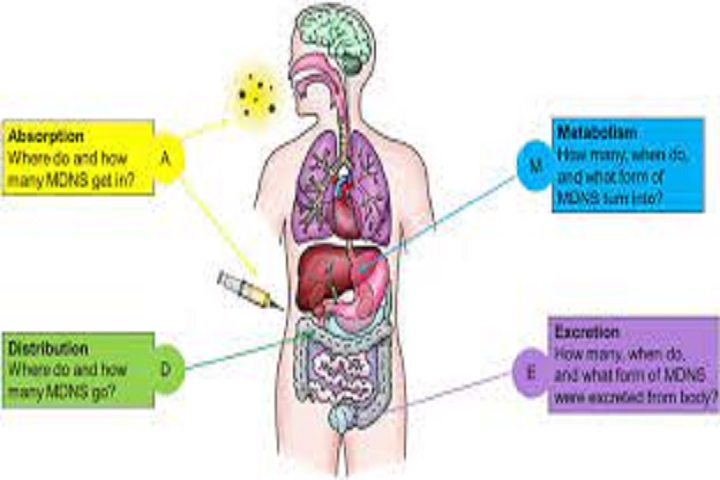
Absorption
Drugs may be given by a variety of routes; the route chosen depends on the desired site of action and the type of drug preparations available. Routes used commonly by the anesthetist include inhalation, intravenous, oral, intramuscular, rectal, epidural, and intrathecal. Other routes, such as transdermal, subcutaneous, and sublingual, also can be used.
The rate and extent of absorption after a particular route of administration depends on both drug and patient factors. Drugs may be given orally for local as well as systemic effects, for example, oral vancomycin used to treat pseudomembranous colitis is acting locally; antacids also act locally in the stomach. In such cases, systemic absorption may result in unwanted side effects.
Intravenous administration provides a direct, and therefore more reliable, route of systemic drug delivery. No absorption is required, so plasma levels are independent of such factors as gastrointestinal (GI) absorption and adequate skin or muscle perfusion. However, there are disadvantages to using this route.
Pharmacological preparations for intravenous therapy are generally more expensive than the corresponding oral medications, and the initially high plasma level achieved with some drugs may cause undesirable side effects. In addition, if central venous access is used, this carries its own risks. Nevertheless, most drugs used in intensive care are given by intravenous infusion this way.
Oral
After oral administration, absorption must take place through the gut mucosa. For drugs without specific transport mechanisms, only unionized drugs pass readily through the lipid membranes of the gut. Because the pH of the GI tract varies along its length, the physicochemical properties of the drug will determine from which part of the GI tract the drug is absorbed.
Acidic drugs (e.g. aspirin) are unionized in the highly acidic medium of the stomach and therefore are absorbed more rapidly than basic drugs. Although weak bases (e.g. propranolol) are ionized in the stomach, they are relatively unionized in the duodenum, so are absorbed from this site. The salts of permanently charged drugs (e.g. vecuronium, glycopyrrolate) remain ionized at all times and are therefore not absorbed from the GI tract.
In practice, even acidic drugs are predominantly absorbed from the small bowel, as the surface area for absorption is so much greater due to the presence of mucosal villi. However, acidic drugs, such as aspirin, have some advantages over basic drugs in that absorption is initially rapid, giving a shorter time of onset from ingestion, and will continue even in the presence of GI tract stasis.
Bioavailability
Bioavailability is generally defined as the fraction of a drug dose reaching the systemic circulation, compared with the same dose given intravenously (i.v.). In general, the oral route has the lowest bioavailability of any route of administration. Bioavailability can be found from the ratio of the areas under the concentration-time curves for an identical bolus dose given both orally and intravenously.
Factors influencing bioavailability
Pharmaceutical preparation – the way in which a drug is formulated affects its rate of absorption. If a drug is presented with small particle size or as a liquid, dispersion is rapid. If the particle size is large, or binding agents prevent drug dissolution in the stomach (e.g. enteric-coated preparations), absorption may be delayed.
Physicochemical interactions – other drugs or food may interact and inactivate or bind the drug in question (e.g. the absorption of tetracyclines is reduced by the concurrent administration of Ca2+ such as in milk).
Patient factors – various patient factors affect the absorption of a drug. The presence of congenital or acquired malabsorption syndromes, such as coeliac disease or tropical sprue, will affect absorption, and gastric stasis, whether as a result of trauma or drugs, slows the transit time through the gut.
Pharmacokinetic interactions and first-pass metabolism – drugs absorbed from the gut (with the exception of the buccal and rectal mucosa) pass via the portal
 TRUTHREVIEWERS
TRUTHREVIEWERS